The Unseen Grief: Why Perinatal Loss Is Profoundly Different for Neurodivergent Parents
As a counselor specializing in trauma and neurodivergence, I’ve witnessed firsthand the universal pain of perinatal loss. However, grief is not reserved solely for the death of a baby; it is also found in the quiet, heavy loss of what could have been.
For neurodivergent people, including those on the autism spectrum or living with ADHD, the grief process often begins long before a physical loss. It is the grief of a failed IVF journey, the shattering of hope after years of trying to conceive, or the birth trauma that stems from a total loss of choice during birthing. When the birth experience you prepared for is replaced by a clinical crisis, the impact on perinatal mental health during the postpartum period is profound.
The Intersection between Grief and Neurodivergence
The Window of Tolerance
For individuals who identify as neurodivergent, the experience of loss; including miscarriage, stillbirth, and neonatal death; is often compounded by a nervous system that is already highly reactive and hypersensitive.
According to Polyvagal Theory, individuals with a history of trauma or complex processing differences often have their "neural reactions retuned towards a defensive bias." This means the common experience of "shock and disbelief" typical of early grief can persist as a prolonged state of sympathetic "fight or flight" (anxiety/rage) or a parasympathetic "freeze" (shutdown/depression).
The goal of specialist support is to help parents stay within their window of tolerance. For neurodivergent parents, this window may be narrower due to sensory sensitivities. Cues of safety—such as quiet environments, melodic vocalizations, and compassionate interactions—are essential antidotes. Through a subconscious process called neuroception, the autonomic nervous system detects these cues. If the healthcare environment feels dismissive, and does aknowledge the special support needs, it can exacerbate the "social death" of grief, where the parent feels emotionally unseen, leading to worse mental health outcomes.
Intergenerational and Developmental Impact
The neurodivergent experience of perinatal trauma can have long-lasting, embodied effects. For example, birth-related difficulties like anesthesia, inductions, or emergency surgery result in physiological stress for both mother and baby.
In some cases, a child’s later struggle with panic or "life-protecting rage" can be linked to somatic memory from a traumatic birth. This suggests that the impact of negative pregnancy outcomes or birth trauma manifests as developmental interruptions that require a deeply trauma-informed approach to supporting families, through pregnancy and postpartum.
That is why a Doula that understands the specific needs of those that have ADHD, Dyslexia, dyspraxia or autistic women, is a valuable resource while navigating pregnancy and birth. Making a plan that includes special accommodations to avoid sensory overload, or serving as someone to guide and interpret the medical terms and instructions in real time, someone that can advocate for your needs and can help with preparing scrips for common questions and what topics are “green, yellow, red light”so you are not caught off guard and protect your emotional health or and even to provide support during a pregnancy loss.
When Connection Fades: The "Distant" Reality of Trauma through perinatal experiences
Many of my clients describe a terrifying sense of being "cut off" from reality. Even with loved ones nearby, that have also experienced the loss of a loved one, they feel distant from everything and everyone—as if they are watching their life through a thick pane of glass. One woman described it as "losing the frequency" to connect with others.
Another woman shared that she deep dived into her special interest as a coping mechanism and was later confronted by her partner about her perceived lack of interest, which made her spiral into shame and self-doubt.
While someone else shared that the inability to see her baby and to say goodbye, made it impossible for her to mentally process the event and gain closure, prolonging her grief even more.
A common story that is shared with me is how people on the autism spectrum often feel reluctance to disclose their diagnosis because they fear stigma or being labeled as unfit, which stopped them from getting adjustments during pregnancy and parenting leading to traumatics birth or postnatal experiences.
A shared experience of many parents is the feeling that their grief is invisible or socially “unauthorized,” especially in cases of early loss. This often leads to withdrawal, self-silencing, and a sense of walking a solitary path. The need for pregnancy and infant loss awareness remains critical, and for many neurodivergent people, who may already struggle to navigate societal norms, the impact is even greater, often discouraging them from seeking support.
Part of the healing journey is not just "talking about it," but slowly bringing back that physiological capacity to connect. This is why co-regulation with a counselor is vital. We provide a safe space, tailored psychoeducation, validation, while supporting neurodivergent individuals in building internal resources.
Therapeutic Frameworks: ACT and Sensory Interventions for supporting neurodivergent families
The "Observer Self" (ACT)
For those who struggle with traditional "talk therapy," Acceptance and Commitment Therapy (ACT) and somatic interventions offer a path forward, for bereaved families.
ACT (Acceptance and Commitment Therapy): Rather than trying to "fix" the pain, ACT encourages giving space to negative emotions, without trying to change, avoid or surpress them. This does not mean that we need to approve of the loss, but rather recognizing and acknowledging that the pain exists. When we cease to fight against the negative feelings, we can reduce the energy spent in this internal fight and use the resources to heal. To achieve this we use
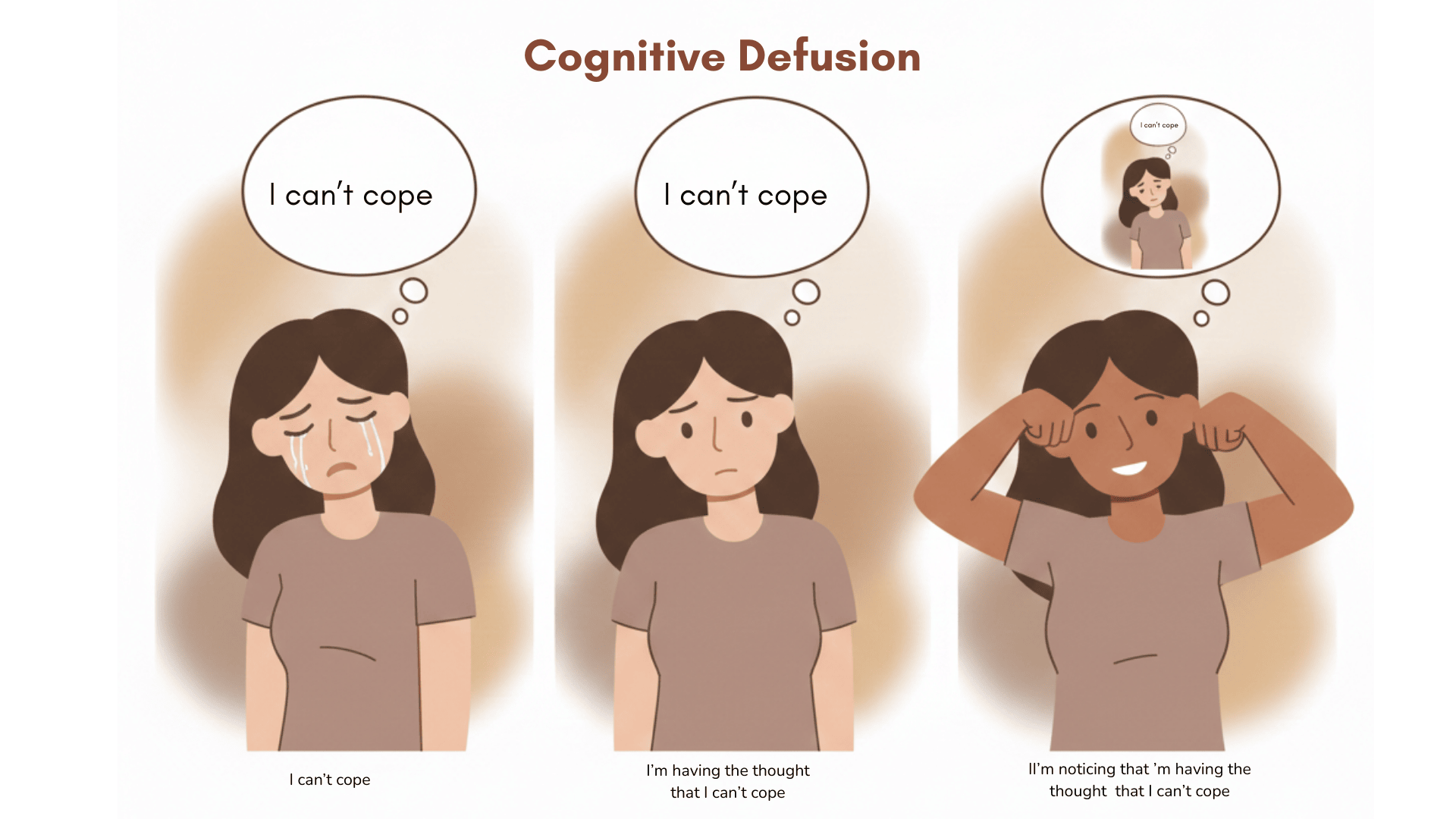
Cognitive Defusion, creating distance and reframing overwhelming thoughts (e.g., "I am noticing the thought that I am not coping" instead of "I cant cope").
Sensing and Somatic Work: Non-verbal approaches like rhythmic movements or stimming to help regulate the nervous system.
Rituals and Symbols: Because loss often lacks "shared stories," we use identity work to help break the silence and give space for healing. Using art, writing letters to the baby you never met, or meaningful objects helps families give the loss a tangible place in their new life.
The Cognitive Load of "Miscarriage admin" while seeking support
Grieving involves a staggering number of tasks. For someone with executive functioning challenges, this load can be completely overwhelming. When a parent misses a medical appointment or an appointment with a medical provider like a midwife, or is completely unable to make arrangements for the funeral or tend to paperwork, it is often misjudged as a lack of engagement. In reality, it is the intersection of profound perinatal loss and executive shutdown. Supporting families effectively means providing practical help that allows accommodations for the cognitive and sensory experiences of autistic mothers, rather than judgment, that leads to added shame and grief.
A Call for Compassionate Accommodation
ADHD and other neurodevelopmental conditions are associated with higher rates of anxiety, depression, trauma, and less adaptive coping, so Supporting neurodivergent parents through loss, whether it is a miscarriage, a stillbirth, or the loss of the birth experience you deserved, requires us to move beyond generic sympathy, tailoring our support so it can accommodate the specific needs like sensory processing of autistic individuals.
By recognizing these neurodivergent realities, we don't just offer better maternity care; we offer a path back to connection and safety, improving the health and wellbeing, during the perinatal period, for the whole family.