Postpartum support for neurodivergent parents: The Invisible Fourth Trimester, and Why We Need a Map
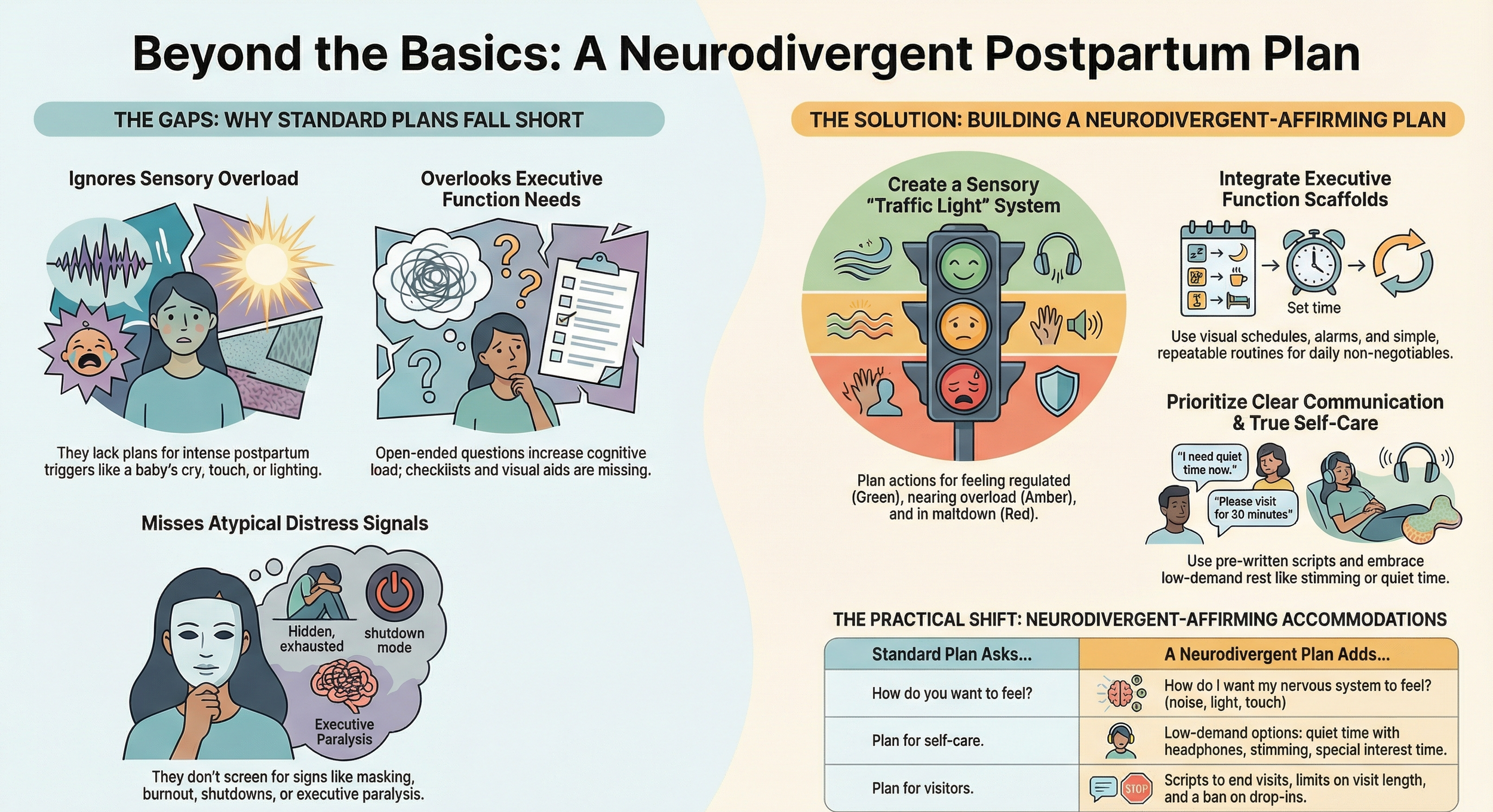
Everyone talks about the birth plan, but what about the after plan? For neurodivergent parents, the early postpartum period, often called the "fourth trimester", isn't just challenging; it can be overwhelming, unpredictable, and even destabilising without intentional preparation.
Imagine navigating a new city with a complex, evolving map, except you're sleep-deprived, hormonally charged, recovering from a major physical event, and trying to decipher a tiny human's needs, while also navigating the new experiences of infant feeding. Now imagine doing that when your brain thrives on predictability, routine, clear instructions, and sensory regulation. Suddenly, "winging it" isn't just difficult; it's a recipe for burnout.
This isn't about perfection; it's about building a personalised safety net that honours your unique brain.
Why Postpartum Planning Matters: Addressing perinatal experiences for ADHD and autistic parents
The statistics paint a clear picture: neurodivergent women often face unique challenges and adverse health outcomes during childbirth and postnatal experiences that recognise the urgent need for inclusive, tailored support and planning for neurodivergent families.
Higher Risk of Perinatal Mood and Anxiety Disorders (PMADs):
The unique experiences of neurodivergent expectant women during pregnancy, birth and early parenting, due to a lack of neurodiversity-affirming care, often lead to poorer health outcomes. A recent example is the 2024 systematic review “A Systematic Review of the Perinatal Mental Health Outcomes of Women with Neurodevelopmental Disorders,” studies included in this review found that neurodivergent mothers (including those with adhd and autism and other neurodevelopmental conditions) consistently showed higher levels of perinatal depression and/or anxiety symptoms than neurotypical women, indicating an elevated risk of Perinatal Mood and Anxiety Disorders.
Sensory Overload & Meltdowns:
Sensory experiences in healthcare systems (noise, lights, touch and procedures) during pregnancy and birth are frequently described by neurodivergent people as overwhelming and can precipitate or exacerbate birth trauma, unless sensory‑adapted, trauma-informed maternity care is provided. This lived experience during birth can already set up autistic and adhd parents at a disadvantage when dealing with the constant demands of a newborn, unpredictable cries, touch, smells, lack of sleep, which are typical of early parenthood. This constant and intense sensory overload can increase the likelihood of meltdowns or shutdowns.
Executive Function Demands:
Experiences in the early postpartum are comparable to an executive function marathon: meal prep, appointments, tracking feeds, sleep deprivation, and household management. For those parents with adhd, these demands can quickly lead to overwhelm, dysfunction, decision paralysis, and self-criticism.
Trauma Re-enactment:
As mentioned before, birth trauma is unfortunately more common for neurodivergent individuals due to communication difficulties, sensory sensitivities, and feeling unheard. Without postpartum support that caters for the needs of women with adhd and autistic mothers, a chaotic postpartum period can inadvertently re-trigger past trauma responses.
Masking & Burnout:
Many parents mask their struggles to fit societal expectations, leading to severe burnout and delaying seeking care during the perinatal period. A plan acknowledges these unique needs of neurodivergent people upfront.
When the Plan Saves the Day
A neuro-affirming postpartum care plan can make a tangible difference, as shared in the examples below:
The Mealtime Meltdown:
Without a plan: Sarah, an ADHD mom, found herself staring blankly into the fridge at 5 pm, baby screaming, feeling utterly defeated because she hadn't eaten all day. Her partner, also overwhelmed, brought home fast food again, leading to guilt and another executive function crash trying to find utensils.
With a plan: Before birth, Sarah and her partner pre-arranged a meal delivery service for the first two weeks and batch-cooked freezer meals. They bought a month's supply of disposable plates and cutlery. When 5 pm hit, a simple text to the delivery service or a pre-labelled freezer meal meant one less decision, one less overwhelm, and nourished bodies.
The Sensory Storm:
Without a plan: David, an autistic father, felt increasingly agitated by the constant baby noises and bright lights in their living room. He'd retreat to the bedroom, feeling guilty about not helping, but unable to articulate his sensory overload. His partner felt abandoned.
With a plan: David and his partner discussed sensory needs before birth. They designated a "quiet zone" in their home, invested in noise-cancelling headphones for David, and agreed on a visual cue system (e.g., a coloured card on the door) to signal when he needed a sensory break. They also stocked up on baby-safe dim lights and soft blankets.
The Support System Struggle:
Without a plan: Maria, who experiences anxiety, felt overwhelmed by well-meaning visitors who stayed too long, asked too many questions, and didn't help. She'd mask her discomfort, then crash once they left, resenting the intrusions.
With a plan: Maria and her partner created a "Visitor Protocol" for friends and family: specific visiting hours, a "task list" on the fridge (e.g., "wash bottles," "take out bins"), and a pre-written text message to send when they needed alone time. They also identified social support and designated one or two trusted friends to call when they needed someone who could hold the baby while Maria showered, no conversation required.
Building Your Neuro-Affirming Postpartum Plan: Key Elements for better support
A robust postpartum plan isn't about rigidity; it's about supporting neurodivergent needs by reducing cognitive load, managing sensory input, and securing support, allowing for positive experiences in early postpartum.
support groups Audit:
Who can cook? Who can clean? Who can just listen without judgment?
Identify trusted friends/family for specific, actionable tasks.
Consider professional support: a neuro-affirming doula, therapist, health professional or postpartum helper.
Sensory Care Environment Design:
What are your "green zone" sensory preferences (dim lights, quiet, soft textures)?
What are your "red zone" triggers (loud noises, strong smells, too much touch)?
Plan for noise-cancelling headphones, dimmable lights, comfortable clothing, unscented products. Create a designated "safe space" for overwhelm.
Meal & Household Management:
Batch cooking, meal delivery, and grocery delivery services.
Disposable plates/cutlery.
A "good enough" standard for household chores. Delegate ruthlessly.
Self-Care & Regulation Strategies:
Non-negotiable moments for deep pressure, quiet time, or stimming.
Scheduled breaks. Short, frequent moments of regulation are more sustainable than waiting for a full meltdown.
Therapy/coaching appointments pre-booked.
Communication Protocol:
Use the pre-written scripts from the infographic to end visits early or signal a need for quiet time. True self-care for the neurodivergent brain often looks like low-demand rest, such as stimming or using noise-cancelling headphones.
"Just In Case" Contingency plan
What if a plan falls apart? Who can provide inclusive care? Who do you call? What's your backup meal/support?
Empowering Your Unique Parenting Journey
Postpartum planning isn't a luxury; it's a necessity, especially for those with or without a formal diagnosis, navigating neurodiversity in a world not always built for their brains. By proactively addressing perinatal needs, like sensory inclusive spaces, executive function challenges, and communication styles, you're not just surviving; you're building resilience and creating a foundation for an empowered, authentic, and truly neuro-affirming postpartum experiences.
Your unique brain is a superpower; let's plan to protect it.